Understanding the connection between nerve and pain is crucial for effectively managing and treating various types of pain conditions. When a nerve is injured or compressed, it can send signals to the brain that are interpreted as pain. This intricate relationship between the nervous system and pain perception is a complex area of study in the field of medicine.
Recent research has shown that chronic pain conditions, such as neuropathic pain, are directly related to abnormal nerve function. By understanding how nerves communicate pain signals to the brain, healthcare professionals can develop targeted treatments to alleviate pain and improve the quality of life for patients suffering from these conditions.
Understanding the Link Between Nerve and Pain
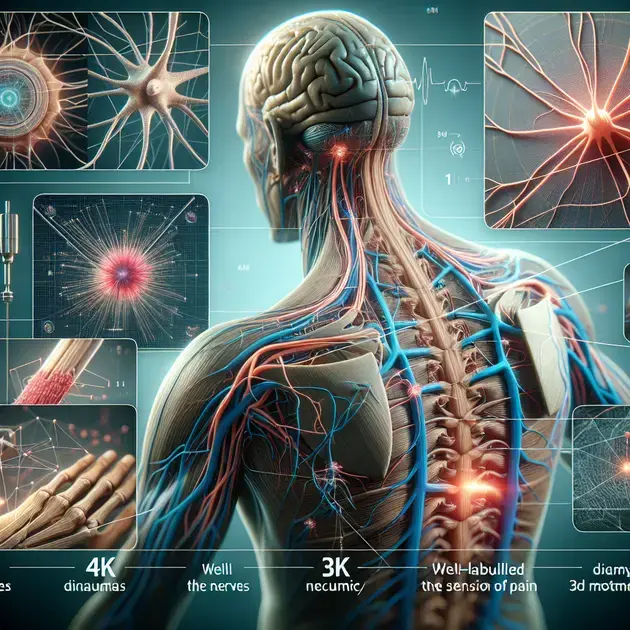
Understanding the connection between nerves and pain is crucial for managing and treating pain effectively. Nerves play a key role in transmitting pain signals from the body to the brain, where pain is perceived. To comprehend this link, it is essential to delve into the basics of the nervous system and its functions in pain perception.
The nervous system is divided into the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS includes the brain and spinal cord, while the PNS comprises the nerves that extend throughout the body. When there is tissue damage or injury, specialized nerve receptors called nociceptors detect these harmful stimuli and send signals to the brain, resulting in the sensation of pain.
To understand the link between nerve and pain, individuals can explore resources such as reputable medical websites like WebMD or Healthline. These websites offer detailed articles and diagrams explaining the process of pain perception and how nerves play a vital role in this mechanism. By educating oneself on the intricacies of the nervous system, individuals can gain insights into how pain manifests and strategies for pain management.
Additionally, educational apps like Complete Anatomy provide interactive 3D models of the human body’s nervous system, allowing users to visualize how nerves transmit pain signals. By examining these visual representations and engaging with the app’s educational content, individuals can enhance their understanding of the intricate connection between nerves and pain.
By grasping the link between nerve function and pain perception, individuals can advocate for personalized pain management strategies that target the underlying causes of pain. Through education and exploration of resources, individuals can empower themselves to make informed decisions about their pain treatment.
The Complex Interaction of Nervous System and Pain Perception
The interaction between the nervous system and pain perception is a multifaceted process that involves various neurotransmitters, receptors, and brain regions. Understanding this complexity is essential for developing effective interventions for pain management. One key aspect of this interaction is the role of neurotransmitters in modulating pain signals within the nervous system.
Neurotransmitters such as serotonin, dopamine, and endorphins play crucial roles in regulating pain perception. These chemicals act on specific receptors in the nervous system to either amplify or inhibit pain signals. For example, endorphins, also known as “feel-good” hormones, can bind to opioid receptors in the brain and spinal cord, reducing the perception of pain.
Exploring scientific journals like Pain and The Journal of Neuroscience can provide valuable insights into the complex interaction between the nervous system and pain perception. These publications feature cutting-edge research on the neurobiology of pain and the latest discoveries in pain management strategies.
Mobile apps like NeuroNation offer brain training exercises that can help individuals improve cognitive functions related to pain perception. By engaging in neuroplasticity-focused activities, users can enhance their brain’s ability to regulate pain signals and mitigate the impact of chronic pain.
By delving into the intricate relationship between the nervous system and pain perception, researchers and healthcare professionals can develop targeted treatments that address the underlying mechanisms of chronic pain. Collaborative efforts in neurology, pain management, and pharmacology are essential for advancing our understanding of this complex interaction and improving patient outcomes.
Targeted Treatments for Chronic Pain: A Focus on Nerve Function
Targeted treatments for chronic pain often involve interventions that specifically address nerve function and transmission of pain signals. By targeting the underlying mechanisms of pain at the nerve level, healthcare providers can offer more personalized and effective pain management strategies for individuals suffering from chronic pain conditions.
One targeted treatment approach for chronic pain is nerve blocks, which involve the injection of local anesthetics or steroids to block nerve signals in specific areas of the body. Nerve blocks can provide temporary relief from pain and help healthcare providers identify the source of pain for further treatment.
Websites like PainDoctor.com offer extensive information on different types of nerve blocks, their applications, and potential benefits for chronic pain conditions. Patients can access articles, videos, and patient testimonials to gain insights into how nerve blocks can be used as targeted treatments for managing chronic pain.
Another targeted treatment option for chronic pain is neurostimulation, which involves the use of implanted devices to deliver electrical impulses to targeted nerves or the spinal cord. Neurostimulation techniques, such as spinal cord stimulation, can modulate pain signals and provide relief for individuals with persistent and treatment-resistant chronic pain.
Healthcare professionals can leverage resources like the International Neuromodulation Society website to stay updated on the latest advancements in neurostimulation technologies and evidence-based practices for chronic pain management. By incorporating targeted treatments that focus on nerve function, healthcare providers can offer comprehensive care plans that address the unique needs of patients with chronic pain.
To develop each subtitle with the corresponding HTML tags, follow these steps:
1. **The Role of Neural Pathways in Pain Management**:
Neural pathways play a crucial role in the perception and transmission of pain signals in the human body. These pathways are a complex network of nerves and structures that carry sensory information from the site of pain to the brain, where it is processed and interpreted. Understanding how neural pathways function is essential for effective pain management strategies.
When an individual experiences pain, specialized nerve receptors called nociceptors send signals through these neural pathways to the brain, alerting it to potential tissue damage or injury. Different types of neural pathways are involved in transmitting various types of pain, such as acute pain from injuries or chronic pain from conditions like arthritis.
By studying and mapping these neural pathways, healthcare professionals can develop targeted interventions to modulate pain signals and provide relief to patients. Techniques like nerve blocks, spinal cord stimulation, or medication targeting specific neurotransmitters can disrupt or modulate pain signals along these pathways, offering pain management solutions.
Overall, the role of neural pathways in pain management is central to understanding how pain is perceived and processed in the body. By targeting these pathways with precise interventions, healthcare providers can offer effective relief and improve the quality of life for individuals experiencing pain.
As research continues to advance in the field of pain management, further insights into the intricacies of neural pathways and their modulation will pave the way for more efficient and personalized treatment strategies for various pain conditions.
2. **Exploring the Role of Neurotransmitters in Pain Signals**:
Neurotransmitters are essential chemical messengers that play a crucial role in transmitting pain signals within the nervous system. These neurotransmitters are released by nerve cells in response to stimuli, facilitating the communication between nerve cells and influencing the perception of pain in the brain.
Specific neurotransmitters, such as serotonin, dopamine, and endorphins, are known to modulate pain signals and regulate pain sensitivity levels. Imbalances in these neurotransmitters can lead to alterations in pain perception, contributing to conditions like chronic pain syndromes or neuropathic pain.
By exploring the role of neurotransmitters in pain signals, researchers can gain valuable insights into the mechanisms underlying different types of pain and develop targeted therapies that address neurotransmitter imbalances. Medications that target specific neurotransmitter pathways, such as serotonin reuptake inhibitors or opioid agonists, can help manage pain and improve the quality of life for individuals experiencing chronic or acute pain.
Understanding how neurotransmitters interact within the neural pathways involved in pain transmission is key to developing novel approaches to pain management. By targeting specific neurotransmitter systems, healthcare providers can tailor treatment strategies to address the unique biochemical profiles of patients and offer more effective pain relief solutions.
As research continues to unravel the complexities of neurotransmitter interactions in pain signaling, new therapeutic opportunities emerge, leading to innovative strategies for pain management and enhanced patient outcomes.
Conclusion
Neural pathways play a pivotal role in how pain signals are perceived and transmitted throughout the human body. These intricate networks of nerves and structures form the foundation for understanding and effectively managing pain. By comprehending the mechanisms of neural pathways, healthcare professionals can implement targeted interventions to modulate pain signals and offer relief to patients. Techniques like nerve blocks and spinal cord stimulation, as well as medications targeting specific neurotransmitters, can disrupt or modulate pain signals, providing tailored solutions for pain management.
Understanding the significance of neurotransmitters in pain signaling is essential for developing innovative approaches to pain management. These chemical messengers play a vital role in transmitting pain signals within the nervous system, influencing the perception of pain in the brain. By exploring the role of neurotransmitters, researchers can better grasp the underlying mechanisms of different pain types and develop therapies that address neurotransmitter imbalances. Medications targeting specific neurotransmitter pathways offer promising avenues for managing chronic and acute pain, thereby enhancing the quality of life for individuals experiencing pain.
In conclusion, the intricate interplay between neural pathways and neurotransmitters underscores the complexity of pain management. By delving deeper into these mechanisms, healthcare providers can tailor treatment strategies to individual patients’ biochemical profiles, offering more effective and personalized pain relief solutions. Continued research in this field will unveil further insights into pain signaling and provide a foundation for developing advanced treatment strategies, ultimately leading to improved patient outcomes and enhanced quality of life.