Plica syndrome of the knee is a condition that often elicits confusion and debate, even among medical professionals. In this blog, we aim to unravel the mystery surrounding this phenomenon and provide a comprehensive understanding for those affected by it. We will delve into the intricacies of plica syndrome, including its signs and symptoms, explore the variety of treatment options available, and address the prevalent question of why orthopedic surgeons typically shy away from surgical intervention. Informed by Dr. David Guyer, a triple board-certified orthopedic surgeon and expert in sports medicine and regenerative practices, this discussion will illuminate the reasoning behind the cautious approach to surgery and offer insight into alternative measures that may alleviate discomfort effectively. Whether you’re newly diagnosed or seeking to deepen your knowledge, this guide aspires to offer clarity and guidance on navigating plica syndrome.
Understanding Plica Syndrome
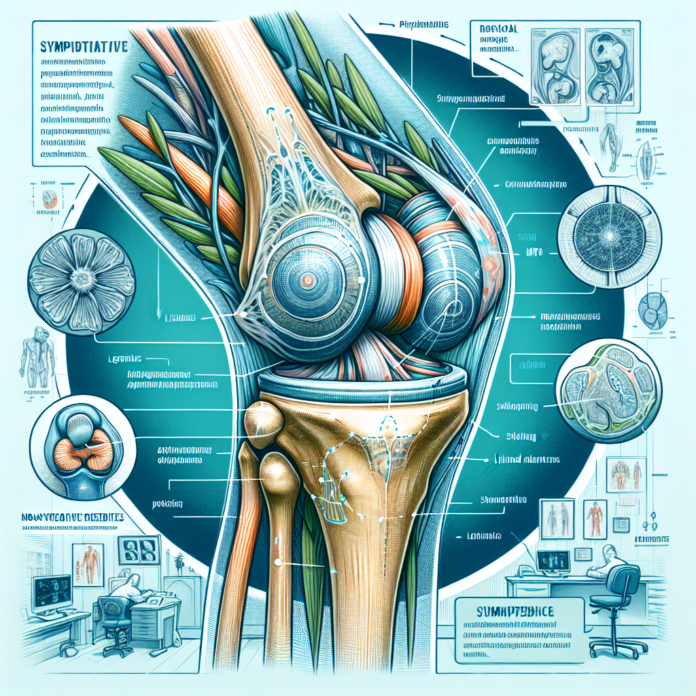
Plica syndrome is characterized by the presence of an extra band of synovial tissue in the knee joint, known as plica. This tissue often lurks silently in the knee, with the majority of individuals being completely unaware of its existence. For some, however, this seemingly innocuous tissue can become inflamed, leading to discomfort and mechanical symptoms like a snapping sensation during knee movement.
The condition frequently manifests when the knee experiences trauma or repeated stress, causing the synovial tissue to become irritated and inflamed. As Dr. David Guyer points out, this syndrome can be quite common, affecting roughly 5% to 25% of the population. Despite the prevalence of plica tissue, only a small fraction of individuals actually experience symptoms severe enough to warrant medical attention.
Symptoms of Plica Syndrome
- Pain: Pain localized to the anterior part of the knee or around the patella is common. It might especially be felt while climbing stairs or after prolonged periods of sitting or bending the knee.
- Snapping Sensation: One of the hallmark symptoms is a snapping or clicking sensation in the knee during movement, which can be quite discomforting.
- Swelling or Tenderness: Some patients experience swelling around the knee joint or tenderness upon palpation along the plica’s pathway.
Often, plica syndrome is diagnosed through a thorough physical examination, alongside an evaluation of medical history. Although MRI scans can be utilized to rule out other conditions, they might not always clearly showcase the presence of plica, necessitating reliance on more traditional diagnostic measures.
Treatment Approaches
Orthopedic surgeons, like Dr. Guyer, traditionally advocate for conservative treatment methods before considering surgical options:
- Physical Therapy: Engaging in a structured physical therapy regimen is often recommended. Such programs focus on strengthening the muscles around the knee, improving flexibility, and reducing stress on the joint.
- Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to decrease inflammation and alleviate pain.
- Steroid Injections: In cases where inflammation is significant, corticosteroid injections might be employed directly into the knee joint to reduce symptoms effectively.
These non-surgical interventions are aimed at managing the inflammation and improving knee mechanics, often leading to significant improvement in symptoms.
Why Surgeons Tend to Avoid Surgery
The reluctance among orthopedic surgeons to recommend surgery for plica syndrome stems from a few considerations. First, surgery is inherently invasive and carries risks, including infection and prolonged recovery time. The consensus within the orthopedic community, as explained by Dr. Guyer, is that plica tissue very rarely is the primary cause of knee pain. This perception diminishes the rationale for surgical intervention.
Moreover, a significant number of patients with plica syndrome respond favorably to non-surgical interventions. Surgical outcomes can be unpredictable, and there is no guarantee that excising the plica will resolve the pain, especially if the true source of discomfort lies elsewhere.
Where surgery becomes a viable option is in cases where:
- Localized Pain and Confirmation: The pain can be distinctly traced to the plica, with no other underlying conditions identified on diagnostic imaging.
- Failure of Conservative Treatment: Patients have undergone a comprehensive course of conservative management without adequate relief.
- Concurrent Knee Surgery: If a patient is undergoing knee arthroscopy for another condition, and a problematic plica is identified, it may be excised during the procedure.
It’s important to note that the surgical removal of the plica, known as a plica resection, was more common in the past, especially when arthroscopic techniques were first introduced. Advances in understanding knee pathologies and the availability of less invasive treatment modalities have led to a decline in the frequency of this surgery.
Final Thoughts
Navigating plica syndrome can be challenging, but understanding the condition can empower individuals to make informed decisions about their care. The preference for conservative treatment by the medical community underscores the importance of patience and adherence to prescribed non-surgical interventions. As with any medical concern, it is crucial for patients to engage in open dialogue with their healthcare providers to determine the most appropriate treatment path, considering both the risks and potential benefits of surgery.
For those seeking further expertise or struggling with other knee-related injuries, exploring resources such as Dr. Guyer’s “The Arthritis Solution” eBook might provide additional insights into comprehensive treatment strategies beyond the realm of surgery. The path to recovery may not be instantaneous, but with the right support and intervention, individuals with plica syndrome can hope to return to their daily activities with improved comfort and mobility.