A fracture of the medial femoral condyle is a rare but significant injury, especially in adults. In children, however, it’s more frequent due to the nature of their developing bones. This type of fracture can be quite complex and requires careful consideration for treatment and recovery. Understanding when surgical intervention is necessary, the steps involved in the recovery process, and how to manage weight bearing and return to work can help those affected navigate the challenges that come with this injury.
Anatomy of the Medial Femoral Condyle
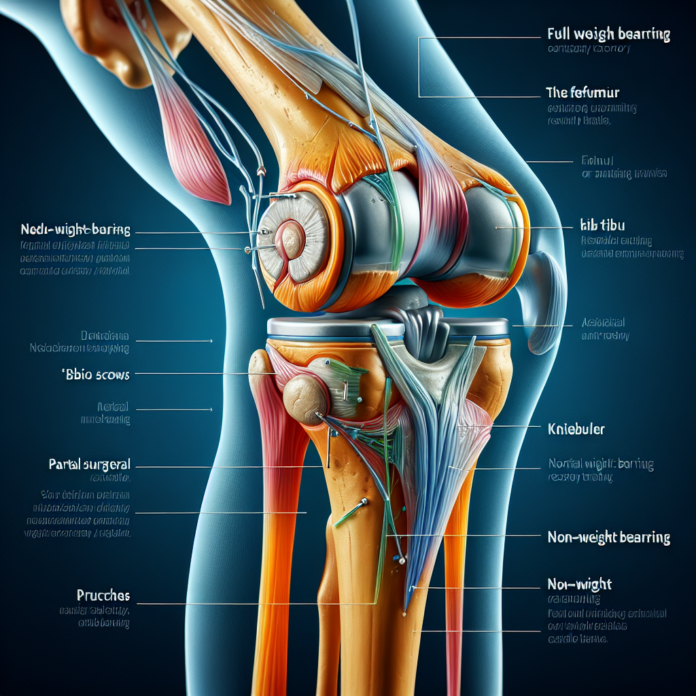
Understanding the anatomy of the medial femoral condyle is crucial to grasp the nature of the injury. The femoral condyles are the rounded ends of the femur (thigh bone) that form part of the knee joint. They articulate with the tibial plateau of the shinbone to allow for smooth movement of the knee. The medial femoral condyle is located on the inner side, closer to the body’s midline.
Pattern of Injury
In adults, the strength of bones compared to ligaments changes, making certain types of injuries more prevalent. For example, while children tend to fracture bones due to their higher flexibility and weaker bones relative to ligaments, adults are more prone to ligament injuries. This difference in injury patterns highlights why medial femoral condyle fractures are less common in adults—it takes considerable traumatic force to cause such a fracture.
When is Surgery Necessary?
When it comes to the decision of whether surgery is necessary for this type of fracture, it often revolves around the alignment of the bone. If the fracture causes a displacement of the bone that affects the knee’s articular cartilage, it can lead to future complications such as arthritis. The cartilage needs to remain smooth to avoid excessive wear and tear during joint movement. If there’s a step-off or misalignment, it can create a rough spot, leading to gradual cartilage deterioration.
Surgical intervention typically involves internal fixation, where a plate and screws are used to hold the bone fragments in place, ensuring they heal correctly. This precise alignment is critical to prevent long-term complications and ensure the smooth function of the knee joint post-recovery.
Recovery Process
The recovery from a medial femoral condyle fracture can be a lengthy and rigorous process. Generally, it takes three to four months for the bone to fully heal. During this time, weight bearing is usually restricted to prevent any displacement that could interfere with the bone’s healing. Typically, an orthopedic surgeon will prescribe limited or non-weight bearing for six to twelve weeks, depending on the specifics of the injury and the patient’s overall health.
Toward the end of the recovery period, partial weight bearing may be introduced. This gradual increase helps in strengthening the muscles surrounding the knee, which may have weakened due to disuse. It’s essential to follow the orthopedic surgeon’s guidance closely to ensure a smooth recovery and to avoid setbacks that could prolong the healing process or require additional surgical intervention.
Returning to Work
Returning to work after a medial femoral condyle fracture depends largely on the nature of one’s job. Those with desk jobs can often resume work relatively quickly, as long as they can manage transportation, potentially with restrictions like crutch use. However, jobs that require standing, walking, or strenuous activity may necessitate a longer recovery period before a full return is possible.
Patients may also explore non-surgical treatments or adjuncts to surgery, such as physical therapy, to aid recovery. These treatments focus on restoring range of motion, maintaining muscle strength, and preventing stiffness in the knee joint.
Conclusion
In summary, a fracture of the medial femoral condyle demands a careful treatment strategy that often involves surgery to ensure proper alignment and healing. Recovery is a multi-step process, requiring patience and adherence to medical advice to prevent complications. For any patient experiencing such an injury, it’s crucial to consult with a healthcare provider who can tailor a treatment and recovery plan to their specific needs. This personalized approach can significantly enhance recovery outcomes and minimize the risk of long-term issues.