A distal biceps tendon rupture can be a daunting injury for those who maintain an active lifestyle, presenting unique challenges in both diagnosis and recovery. In this blog, inspired by the insights of Dr. David Guyer, a triple board-certified orthopedic surgeon, we will delve into the mechanics of this injury, uncover the typical signs and symptoms, and explore the potential pathways to healing. Drawing from questions posed by viewers, we will answer real-life concerns, such as how an everyday activity like throwing a stick could lead to such a rupture. While this blog aims to provide general information and educational content, it highlights the importance of seeking professional medical advice when faced with such injuries. Join us as we uncover the mysteries behind distal biceps tendon rupture and learn how to navigate the road to recovery effectively.
How Does a Distal Biceps Tendon Rupture Occur?
Understanding how a distal biceps tendon rupture occurs is critical, especially for those leading an active lifestyle. This injury can significantly impact your daily activities and overall quality of life, as it disrupts the regular function and aesthetics of your arm.
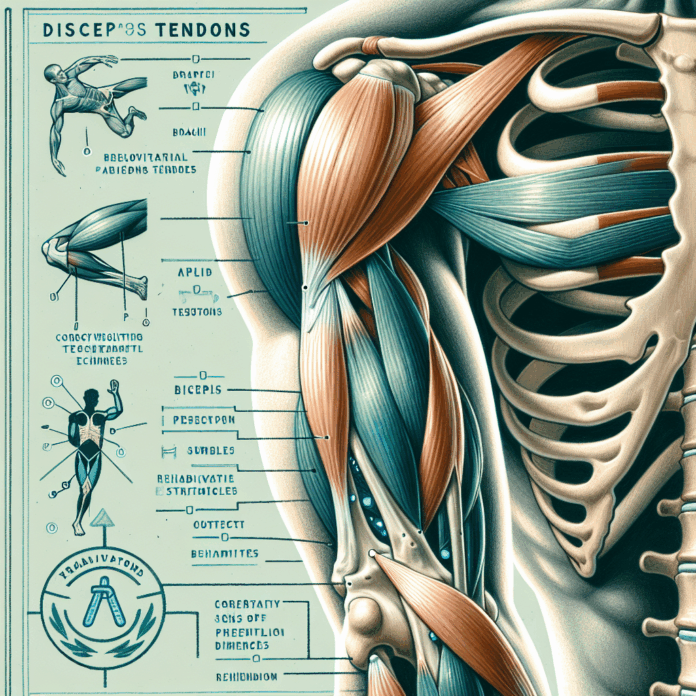
The distal biceps tendon is the pathway through which the biceps muscle attaches to the radius bone in your forearm, just below the elbow. The rupture occurs when there is an unexpected and forceful straightening motion of the elbow while the biceps muscle is contracting. This eccentric loading causes the tendon to detach from the bone.
There are two primary age groups affected by this injury: those in their 30s who are very active and those between 50 and 70. Despite the differences in age and activity levels, the common thread is the abrupt force applied to the biceps under tension. To visualize this, consider someone lifting a heavy object like a sofa. If the object slips and jerks the arm straight, the tension in the biceps increases dramatically, resulting in a potential rupture. Similarly, in a gym setting, a preacher curl gone awry can produce the same outcome if the weight slips, forcing the elbow to extend rapidly.
Recognizing the Symptoms
When a rupture occurs, the symptoms are often immediate and unmistakable:
- Audible Pop: Many individuals report hearing or feeling a pop at the time of injury.
- Bruising and Swelling: Significant bruising quickly emerges in the lower or midsection of the arm around the elbow.
- Popeye Deformity: Named ironically, this refers to the bunched-up appearance of the biceps muscle near the elbow, creating a visibly prominent bulge due to the retracted muscle.
Pathways to Recovery
Prompt attention to these symptoms is critical, as early intervention leads to better outcomes. Surgery is often the recommended treatment for active individuals to restore optimal arm function. Without surgical intervention, the arm may suffer from a permanent loss of strength and endurance, particularly in movements that require turning the forearm or lifting objects.
For those who suspect they’ve suffered a distal biceps tendon rupture, it’s advisable to consult an orthopedic specialist swiftly. Diagnosis can often be made through a physical examination, sometimes avoiding the need for an MRI. However, if surgery is deemed necessary, it should ideally occur within the first few weeks following the injury. Early surgery minimizes complications and offers a more straightforward surgical repair, as the tendon and muscle’s natural elasticity have not yet deteriorated.
Beyond conventional surgical options, Dr. Guyer emphasizes that some individuals may seek non-surgical avenues or wish to learn about alternatives to routine treatments such as cortisone shots. Innovations in regenerative medicine, such as platelet-rich plasma (PRP) therapy or stem cell applications, are becoming more prevalent and offer potential benefits for tendon healing and recovery. Individuals interested in exploring these options should discuss them with their health providers to determine the best individualized treatment plan.
Finally, Dr. Guyer encourages sharing of personal experiences and questions. While it isn’t feasible to offer personalized medical advice in comment sections, engaging in discourse about these injuries raises awareness and understanding, potentially leading to informative content such as video explanations or blog posts like this one.
Conclusion
The key to managing distal biceps tendon ruptures effectively is to act quickly and with informed decision-making. Recognize the symptoms, consult professionals, and explore all available options to ensure a comprehensive approach to recovery. As research and techniques continue to evolve, staying informed and proactive will empower individuals to recover successfully and maintain their active lifestyles.