When a dislocated patella becomes a recurrent issue, it can disrupt not only your performance in sports but also your daily life. Understanding the spectrum of treatment options—from proactive physical therapy and protective bracing to more invasive surgical interventions—is crucial for managing this condition effectively. In this blog, we delve into the strategies to prevent repeated patella dislocations and explore when it might be time to consider surgery. Led by the insights of Dr. David Guyer, a renowned orthopedic surgeon specializing in sports medicine and regenerative techniques, you’ll gain a comprehensive understanding of how to address this common yet challenging injury. Whether you’re an athlete grappling with repeated knee issues or simply seeking to maintain optimum joint health, this guide will equip you with the information needed to make informed decisions about your treatment plan.
Understanding Patella Dislocation
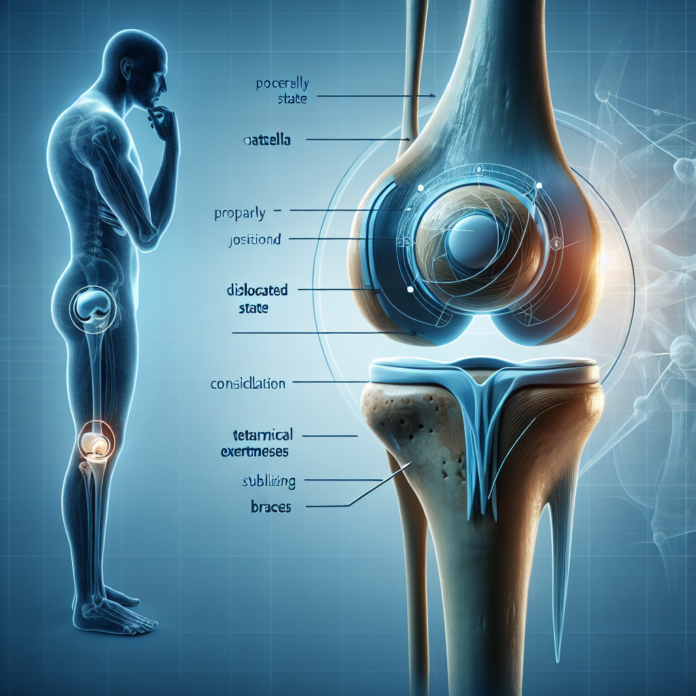
A patella dislocation occurs when the kneecap moves out of its groove on the femur, often to the outside of the knee. This can happen partially (subluxation) or fully. The severity of dislocation can vary, with full dislocations often requiring medical intervention to reposition. Multiple dislocations can indicate underlying issues, such as ligament damage or anatomical variations, which might necessitate more aggressive treatment.
Non-Surgical Treatment Options
Before considering surgery, several non-invasive methods can often succeed in managing and preventing patella dislocations:
- Physical Therapy: A structured physical therapy program can be incredibly beneficial. The goal here is to strengthen the quadriceps, hamstrings, and other supporting muscles around the knee to improve stability. Exercises that enhance the knee’s range of motion and promote muscle balance are generally prioritized.
- Patellar Stabilization Braces: These braces are designed to prevent lateral movement of the kneecap and can be worn during sports activities. While they are not a guaranteed solution for everyone, they can provide additional support and minimize the risk of further dislocations.
Factors Influencing Treatment Success
The success of non-surgical treatments depends on several factors, such as:
- Depth of the Trochlear Groove: A shallow groove can predispose the kneecap to dislocate more easily.
- Ligament Integrity: Damage to the medial patellofemoral ligament (MPFL) can compromise knee stability, making dislocations more frequent.
- Bone Structure: In some cases, a fragment of bone may be displaced during dislocation, complicating treatment.
When Surgery Becomes Necessary
If physical therapy and bracing fail, and dislocations continue, surgical options might be the next course of action. Surgery can address the underlying anatomy or reconstruct damaged structures:
- MPFL Reconstruction: This is the most common surgical procedure for recurrent patella dislocations. It involves reconstructing the MPFL, which acts as a key stabilizer for the kneecap. Surgeons may use a graft (often from a tendon) to restore the ligament’s function and stability.
- Tibial Tubercle Transfer (TTT): In some instances, realigning the extensor mechanism involves moving a portion of the tibial tubercle. This helps correct the tracking of the kneecap, ensuring it stays within the femoral groove during movement.
- Osteotomy: This procedure involves cutting and reshaping bones to correct malalignment and improve joint function.
Post-Surgical Recovery and Rehabilitation
Post-operative care is crucial to ensure a successful recovery. A comprehensive rehabilitation program targets restoring full range of motion, strength, and function. The timeline for returning to sports varies; however, most patients can expect to resume activities approximately 6-12 months post-surgery, depending on the procedure and individual recovery rates.
- Phase 1: Early Recovery: Focuses on reducing swelling, managing pain, and initiating gentle range-of-motion exercises.
- Phase 2: Strengthening: Involves progressive resistance exercises to improve muscle strength around the knee.
- Phase 3: Advanced Functional Training: Prepares the knee for sports-specific movements through dynamic and agility drills.
Conclusion
Recurrent patella dislocations require a comprehensive management approach. While surgery is a viable option for chronic cases, non-surgical interventions should always be attempted first. Partnering with a skilled orthopedic surgeon, like Dr. David Guyer, can open up discussions about all possible routes of treatment. Patella dislocations can be complex, but with tailored care and dedication to rehabilitation, athletes and individuals alike can reclaim their mobility and confidence. Always consult with a healthcare provider to explore the best options for your specific condition.